Integrated Loyalty Systems, ILS, was founded in 2001 by President and Chief Experience Officer, Jake Poore. Our mission to elevate the human side of healthcare is more than just a tagline; it serves as the foundation for everything we do, say, and teach.
In Jake’s own words below, you’ll read the heartbreaking story of his father, Eddie Poore. And perhaps you’ll understand not only what we do, but why we do it.
Here’s Our Why.
“Please, call me Eddie”
Several years back, my dad had a heart attack while on a fishing trip with friends in Michigan. He was rushed to the local emergency department and admitted to the Intensive Care Unit. He needed immediate extensive heart surgery to save his life. I was relieved to find out, after some research, that the hospital had an excellent heart program and very good clinical outcomes.
I took the first flight to Michigan to be with him prior to his surgery. When I arrived, he was in good spirits and joking with the nurses and doctors, who called him, “Mr. Poore.” He gently corrected them by saying, “Please, just call me, Eddie.” They would always reply, “Okay, Eddie. And I’ll make sure everyone else knows that too.”
However, each new nurse or doctor would come in and again address him as “Mr. Poore.” My dad continued to reply, “Just call me, Eddie.”
But they never got it right.
After a while, he became frustrated and a little concerned about his care team’s ability (or inability) to communicate. When a nurse hung a new IV and added some drugs to it, I asked her what it was. She told me it was blood thinner that would help with his heart palpitations.
Each employee also told my dad that prior to surgery, he would need to take off his two gold necklaces. They even offered to take them off right then and send them to security for safe keeping. The necklaces had sentimental value to my father: one was from his mother and one from his deceased wife. He didn’t want them removed! One nurse agreed that the necklaces would be taped to one of his legs during the surgery so that he’d always have them on him. Unfortunately, this was never communicated to other medical-surgical staff.
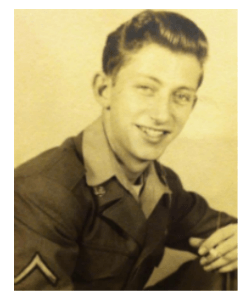
Eddie Poore, Jake’s father
Every time someone new walked into his room, they would kindly suggest that he would have to “take off those gold necklaces.” Finally, my dad lost all patience.
I remember watching his vital signs spike on the monitor above his bed: his blood pressure would rise; his pulse would rise… clearly, there were clinical implications to this poor team communication.
To my dad, the two most important things to him were his good name and his gold necklaces?—?and this team couldn’t get either of these right.
Later, I helped escort my dad to surgery and as I was saying my goodbyes, a nurse said, “Hi, Mr. Poore (not “Eddie”), I’m the nurse anesthetist. Do you know what I’m going to do?” My father replied, “Put me to sleep, I guess.” And she continued, “Yep, that’s right. And I see you have some gold necklaces on, let’s….” While she was still speaking, my father turned back to me with a huge look of fear on his face and said, “Good lord, if they can’t even get these necklaces right, Jake!” That was pretty much the last thing he said on this earth.
(An important note: At 4am, I was in the surgical waiting room and I picked up a newspaper and read that President Clinton had been scheduled to have his heart surgery this same week, but his doctors wanted him to wait an extra few days until the blood thinner had left his body.)
After his surgery the surgeon didn’t even come out to talk to me (a bad sign). He sent one of the nurses out instead.
My father died on the operating table that day.
One of the nurses said, “Your father couldn’t hold his sutures, he just bled out.”
I asked if the blood thinner he was given the night before had anything to do with that.
“Blood thinner? What blood thinner?” she said.
Frustrated, I couldn’t help but say, “You guys couldn’t even communicate the name he wanted to be called or stop asking him about his gold necklaces, maybe you didn’t communicate the blood thinner, either!”
Now, I could have sued them, but I didn’t. It wouldn’t have brought my dad back.
Someone once said, “Patients are experts at what they know and understand and they will make assumptions or judgments on what they don’t know and don’t understand.”
My dad didn’t know how good that hospital was at clinical care, but he was an expert at his name and the importance of his gold necklaces.
Obviously, the loss of my father is an extremely personal and painful memory. I share it with you because I firmly believe that it doesn’t have to be this way.
This is what fuels me. It’s what keeps me up at night. This is my WHY.
My dad’s story is about more than just technical or clinical expertise. It’s about the human side of his experience. The communication between the doctors and nurses on the care team was awful. And the communication between my father and his care team was even worse.
To his doctors and nurses, he was just the ‘4am valve replacement, triple bypass in OR2.’
But to me, he was Eddie Poore.
He was my dad. In healthcare, clinical expertise is a given. Doctors, nurses, and other professionals dedicate years to studying and honing their skills. When patients see their doctor or visit a hospital, clinical excellence is assumed. But clinical excellence is no longer enough. There’s another component to the patient experience, and in the eyes, ears, and nose of the patient, it is just as important. In order to create and deliver exceptional patient experiences, we need to also focus on Service Excellence, or what we call the human side of healthcare.
What does the human side of healthcare look like? Well, it looks like the doctor that walks the patient out of the exam room and back to the reception desk, while answering any last-minute questions (rather than leaving them with unanswered questions and letting them find their own way out). It looks like the housekeeper who offers to change the television channel or retrieve a blanket from the closet for a patient (rather than just sweeping the floor and moving on to the next hospital room.) And it looks like a nurse who communicates to everyone else on the care team about the patient that wants to keep his gold necklaces close to him during surgery (rather than letting that important piece of patient information go in one ear and out the other).
My WHY is to unite professional, medical expertise with human kindness. To bridge the divide between clinical excellence and service excellence. To elevate the human side of healthcare so patients are a little less scared and anxious no matter where they are on the patient experience journey. I’m proud of the work my team and I do. I hope my dad is proud, too.
